Proteins of a feather flock together
Leuven researchers predict how highly similar proteins speed up or halt protein aggregation in Alzheimer’s and other brain diseases
15 March 2022
Different neurodegenerative diseases such as Alzheimer’s and Parkinson’s have one thing in common: one particular protein clumps together, first in one part of the brain, later spreading across other regions, causing increasingly severe symptoms. A research team led by Joost Schymkowitz and Frederic Rousseau at the VIB-KU Leuven Center for Brain & Disease Research has now uncovered how highly similar protein segments can speed up—or more interestingly—thwart this aggregation process, potentially explaining the specific vulnerability of certain brain regions and hinting at potential new ways to develop improved therapeutics.
Protein aggregates as the common thread
What neurodegenerative diseases like Alzheimer’s disease, Parkinson’s disease, ALS and a whole range of others have in common, is the fact that the brains of deceased patients are riddled with protein inclusions.
The identity of the proteins differs, but the sequence of events is similar. Certain proteins become structurally abnormal. Often the culprit proteins fail to fold into their normal configuration; and in this misfolded state, the proteins wreak havoc or lose their normal function, either way disrupting the normal function of brain cells or tissues. The end result: degeneration of certain brain tissues, leading to the diverse disease symptoms featured by neurodegenerative disorders.
Why some protein aggregation starts in a specific brain region—like the region important for memory in Alzheimer’s or the region involved in steering movements in Parkinson’s disease—remains unclear.

Finding the trigger(s)
Frederic Rousseau and Joost Schymkowitz, two professors who jointly lead a lab in Leuven, Belgium, have built their careers studying the biochemistry of how proteins fold and why they misfold. In two new studies, they report how thousands of proteins in our cells bear sequences that resemble the aggregation-prone regions of the culprit proteins involved in Alzheimer’s disease. These ‘third-party proteins’ may play a meaningful part in disease progression, and—more importantly—a potential treatment.
“Aggregation prone regions are short segments with a high propensity to clump together into the sticky structures that essentially make up these disease-related aggregates,” explains Rousseau (VIB-KU Leuven). “The short segments may be part of bigger proteins, and while they typically stick to each other, we wondered whether other proteins with the same or similar regions could also set off this aggregation cascade.”
A grammar for protein aggregation?
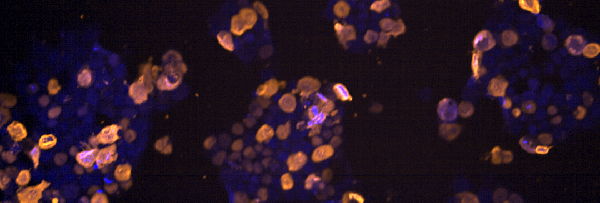
The team set out to look for other proteins containing similar aggregation-prone regions as those found in amyloid beta, the culprit peptide found in Alzheimer’s plaques. Finding many of those, they tested 600 proteins for potential interaction with amyloid beta, explains Katerina Konstantoulea, PhD student in Schymkowitz and Rousseau’s lab: “Thousands of proteins bear sequences that strongly resemble aggregation-prone regions of amyloids, allowing them to interact and either boost or halt the aggregation process.”
To understand why some similar proteins pushed aggregation while others slowed it down, postdoc Nikolaos Louros looked at nearly a hundred aggregation-prone regions, including those for disease-related amyloid beta, tau, and α-synuclein—which aggregate in Alzheimer’s and Parkinson’s disease, respectively.
Using computational methods, Louros modeled all the ways in which changes to the sequence of the aggregation-prone regions would affect their propensity to stick together. “We found that most changes reduced aggregation capacity in some way,” says Louros. “Some by changing the rate of aggregation, others by hindering their spread, still others by modifying the nucleation process or the morphology of the aggregates.”
Designing aggregation-blocking peptides
Using this newly gained information and with tau as an example, Louros and his colleagues tried to design a peptide that would block tau aggregation. In vitro and in cell lines, their synthetic peptide turned out to block tau aggregation and spread five-fold more effectively compared to previous designs, suggesting that this approach could indeed be promising for the development of new therapeutics.
“Our findings indicate that the proteomic background of cells and tissues can modulate the aggregation propensity of culprit proteins, which could explain—at least in part—the selective vulnerability we observe for many of these proteins and diseases,” says Schymkowitz. “Importantly, we can also try to exploit this information to improve therapeutics against several of these neurodegenerative diseases.”

Publications
Heterotypic Amyloid β interactions facilitate amyloid assembly and modify amyloid structure
Konstantoulea et al. EMBO J. 2022
Mapping the sequence specificity of heterotypic amyloid interactions enables the identification of aggregation modifiers
Louros et al. Nature Comms, 2022
Questions from patients
A breakthrough in research is not the same as a breakthrough in medicine. The realizations of VIB researchers can form the basis of new therapies, but the development path still takes years. This can raise a lot of questions. That is why we ask you to please refer questions in your report or article to the email address that VIB makes available for this purpose: patienteninfo@vib.be. Everyone can submit questions concerning this and other medically-oriented research directly to VIB via this address.