Belgian scientists discover how cells protect our skin from inflammatory disease – paving the way for new treatments
Researchers at VIB and Ghent University have uncovered a key mechanism that protects the skin from harmful inflammation
Ghent, 20 October 2025 – Researchers at VIB and Ghent University have uncovered a key mechanism that protects the skin from harmful inflammation. The findings, published in Immunity, could open new avenues for treating chronic skin diseases and other inflammatory disorders.
Our skin is more than just a barrier; it is an active immune organ. When skin cells die in a controlled way, the body usually clears them without issues. But when too many cells die at once or in the wrong way, this process acts like an alarm signal that can trigger conditions such as psoriasis, lupus, or other inflammatory skin diseases.
ATG9A: Cleaning up cells to prevent skin disease
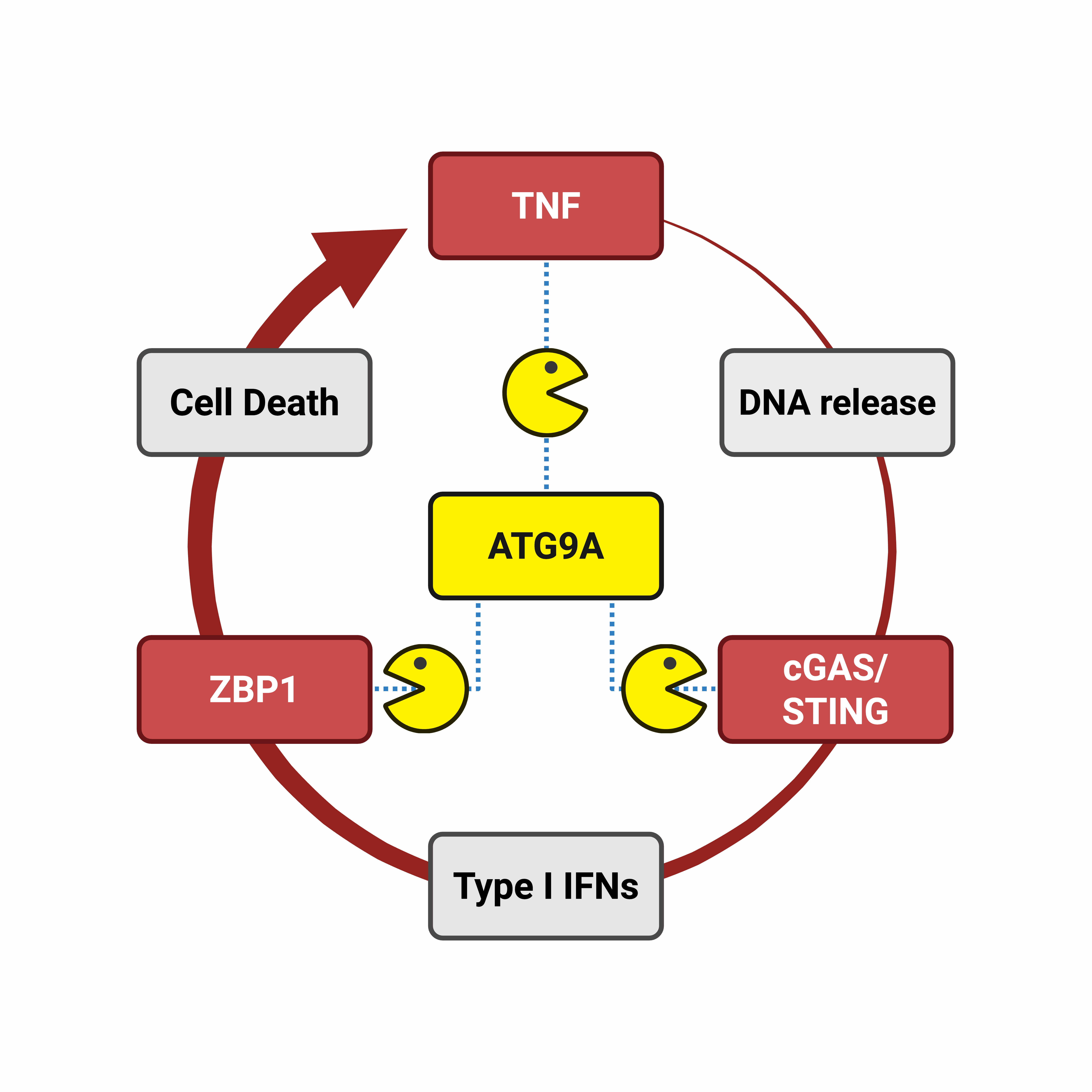
The research team at the VIB-UGent Center for Inflammation Research focused on a protein called ATG9A, which helps cells clean up internal waste through a process known as autophagy. Using advanced mouse models and patient data, they found that ATG9A is crucial for keeping skin cells healthy and preventing excessive inflammation. When ATG9A was missing in skin cells, mice rapidly developed a severe skin disease, driven by a cascade of inflammatory signals. This led to the massive dying of skin cells, which further fueled inflammation and damaged the skin’s protective barrier.
ATG9A helps prevent inflammation by promoting the autophagy-mediated cleanup of inflammatory proteins within skin cells. By removing harmful proteins before they accumulate, ATG9A ensures that inflammatory signals remain under control and the protective barrier is maintained. Interestingly, the research team found that ATG9A mediates this protective function by activating an unconventional, and still largely uncharacterized, form of autophagy.
“ATG9A seems to act as a master repressor of skin inflammation,” said Dr. Dario Priem (VIB-UGent), first author of the study. “By directing inflammatory proteins toward autophagy, ATG9A is capable of shutting down multiple inflammatory pathways.”

A hidden pathway in skin inflammation
Both tumor necrosis factor (TNF) and type I interferons (IFNs) are molecules that play major roles in skin diseases such as psoriasis. Until now, these were seen largely as separate drivers of inflammation.
But this study reveals that TNF and IFNs are tightly connected: TNF can trigger an abnormal IFN response, which in turn amplifies skin damage through a molecule called ZBP1. The researchers discovered that ZBP1 causes excessive death of skin cells when ATG9A is absent, which explains how the skin disease develops.
Because current anti-TNF therapies, commonly used for skin diseases such as psoriasis, can cause serious side effects, targeting the newly discovered TNF–IFN–ZBP1 pathway may offer safer and more precise treatment alternatives. Moreover, blocking this axis could have broader therapeutic potential, as excessive IFN responses are also observed in other TNF-driven inflammatory diseases, such as rheumatoid arthritis and inflammatory bowel disease.
“This discovery not only deepens our understanding of how the immune system is regulated,” says Prof. Mathieu JM Bertrand (VIB-UGent), senior author of the study, “but it also highlights promising new drug targets for patients suffering from skin disease or other chronic inflammatory pathologies.”

Publication
ATG9A-mediated autophagy prevents inflammatory skin disease by limiting TNFR1-driven STING activation and ZBP1-dependent cell death. Priem et al. Immunity, 2025.
Funding
This research was supported by VIB, Ghent University, and FWO.
Gunnar De Winter
About the VIB-UGent Center for Inflammation Research
Inflammation is your body’s response to infection or injury. Normally this is a good defense mechanism. But if something goes wrong with the way this mechanism is controlled, it may result in diseases such as asthma, Crohn's disease or rheumatoid arthritis. The VIB-UGent Center for Inflammation Research investigates the mechanisms that underlie these diseases, they can develop new treatments and improve existing therapies.