Cells that die during inflammation send wound-healing messages
A study by the team of Prof. Kodi Ravichandran (VIB-UGent Center for Inflammation Research) and colleagues found that pyroptosis, a form of programmed cell death traditionally thought to be purely inflammatory, also plays a crucial role in promoting healing and tissue repair. This research, published in Nature, opens new avenues for understanding how our bodies respond to injury and could lead to innovative treatments for wounds and inflammatory diseases.
Dying cells
About a billion cells die in our bodies every day. Most of these cells are killed by a process called apoptosis, which is a form of cellular maintenance that keeps us healthy. However, under the influence of pathogens or inflammatory triggers, cells can die in a process called pyroptosis. As the name suggests (pyro means fire), pyroptosis causes significant inflammation, which helps the body clear infections, but also causes severe tissue damage.
“Cell death by pyroptosis has so far only been regarded as inflammatory and damaging in nature, but our work suggests that, besides tissue-damaging factors, pyroptosis also releases beneficial molecules that encourage wound healing, which could lead to new treatments for dealing with chronic wounds or inflammation,” says Prof. Kodi Ravichandran (VIB-UGent), one of the lead authors of this study.
Inflammation and healing
Whenever we face an injury or infection, our body responds by mounting an immune response, which results in inflammation clearing the infection. However, when the inflammation is not resolved in a timely or controlled manner, there can be excessive tissue damage. Cells undergoing pyroptosis contribute to this inflammation by releasing inflammatory molecules.
However, new research by the team of Prof. Kodi Ravichandran and colleagues finds that these pyroptotic cells also release molecules that can encourage wound healing.
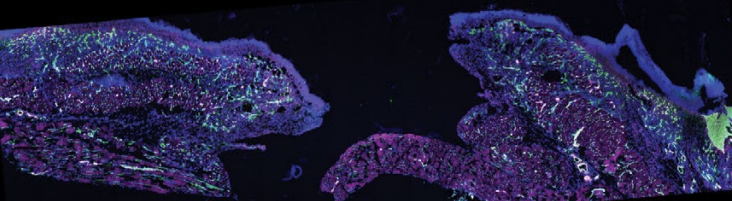
“To our surprise, using cell culture and mouse model systems, the molecules secreted by pyroptotic cells are unique. These molecules induce significant gene expression changes in nearby healthy immune cells (macrophages) that promote healing and tissue repair. So, pyroptosis presses both the accelerator and the brake; on the one hand inflammatory cytokines released from pyroptotic cells cause inflammation, while metabolites and oxylipins in the secretome help the tissue to heal itself” says Dr. Parul Mehrotra, a senior and first author on the study (VIB-UGent, now at Indian Institute of Technology, Delhi).
.png)
Closing wounds
One of the key wound-healing molecules that the researchers identified is prostaglandin E2, known for its role in pain and tissue regeneration.
Dr. Sophia Maschalidi (VIB-UGent), co-first author of this work, says: “Our experiments revealed that the secreted molecules from dying cells, known as the pyroptotic secretome, can significantly boost the body's ability to repair damaged tissues even when inflammatory molecules are present.”
This study suggests that current strategies to develop treatments by blocking pyroptosis may need to be reconsidered. While this can prevent damage, it might also inhibit the release of essential molecules that aid in tissue repair. Instead, the newly identified small molecules and lipids from the pyroptotic secretome could be harnessed to develop new therapies, offering new hope for patients suffering from chronic wounds or inflammatory diseases.
.png)
Funding
This research was supported by the FWO, the Special Research Fund UGent, ERC, BJC Investigator Funds, LEO Foundation EMEA Award, Priority 2030 Federal Academic Leadership Program of the Russian Federation, EMBO, Boehringer Ingelheim, and the Lawrence C. Pakula, MD IBD Innovation Fund.
Publication
Oxylipins and metabolites from pyroptotic cells act as promoters of tissue repair. Mehrotra, Maschalidi, et al. Nature, 2024. DOI: 10.1038/s41586-024-07585-9
.png)


