Researchers map cell composition of metastatic melanoma and identify cause of immunotherapy resistance
Targeting mesenchymal-like melanoma cells could instigate immunotherapy response
Leuven, 9 January 2023 – A group of researchers, led by Professor Jean-Christophe Marine at the VIB-KU Leuven Center for Cancer Biology, and Medical Oncologist Professor Oliver Bechter from UZ Leuven developed a potential new strategy to enable immunotherapy in melanoma patients who currently do not respond to it properly. Using advanced single-cell technologies, they found a specific group of cancer cells that confers resistance to immunotherapy. The team then created a treatment strategy to get rid of these cells, significantly boosting the effectiveness of immunotherapy in preclinical models. The findings of this research have just been published in Cell.
Immunotherapy has emerged as a ground-breaking method for treating cancer, harnessing the body’s own immune system to combat tumors. Recent advances in this area have shown promising results, particularly for patients with advanced skin cancers like melanoma. However, a significant hurdle remains. Less than 50% of melanoma patients respond well to immunotherapy.
The reasons for this resistance are not fully understood, prompting a team of researchers led by Professor Jean-Christophe Marine (VIB-KU Leuven Center for Cancer Biology) to take advantage of a new set of tools allowing an in-depth dissection of the tumor ecosystem at an unprecedented level of detail. This tour de force, supported by the VIB Grand Challenges Program and conducted in collaboration with Professor Oliver Bechter and Professor Francesca Bosisio of UZ Leuven, aimed to uncover the underlying factors contributing to immunotherapy resistance.
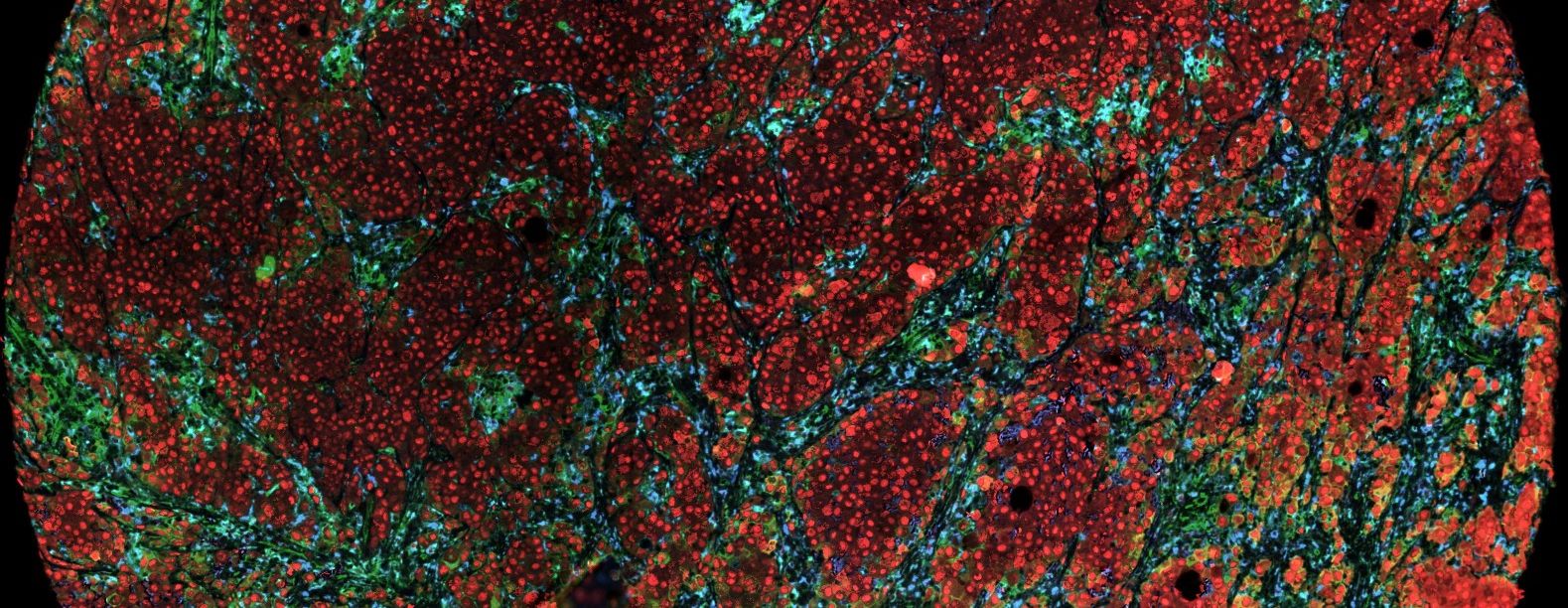
Drawing the map of a melanoma tumor
As a first step, the research team thoroughly analyzed every cancer cell within melanoma lesions obtained from over 20 patients. Using cutting-edge single-cell and spatial technologies, they successfully characterized each individual cancer cell and mapped its precise location within the intricate architecture of the tumor.
Joanna Pozniak (Marine Lab), Ewout Landeloos (Marine Lab) and Dennis Pedri (Marine/Annaert Lab), co-first authors of the paper: "Thanks to close collaboration with UZ Leuven, we could use samples in a longitudinal study, focusing on melanoma patients undergoing immune checkpoint blockade (ICB) therapy, the standard therapy for most melanoma patients. More specifically, we collected biopsies from patients both before initiating treatments and 3 weeks after. Through single-cell RNA sequencing data analysis, we gained detailed insights into the cellular composition of melanoma lesions and their behavior during treatment.
Through this process, the team generated a high-resolution map for each tumor. Their findings revealed that melanomas consist of a diverse array of cancer cells, each exhibiting distinct characteristics. Notably, the unique traits of each cell appeared to be influenced by its location within the tumor and by how it communicated with neighboring cells.

Getting from A to B
With a detailed map of melanoma tumors in hand, the researchers delved into identifying the cell types associated with immunotherapy resistance. Surprisingly, mesenchymal-like cell types, a subset resembling stem cells, turned out to be both quite rare and indicative of a diminished immunotherapy response. The team concluded that these mesenchymal-like melanoma cells possess a remarkable ability to elude immune attacks and potentially promote an environment that compromises the activity of the immune system. In doing so, they contribute to treatment resistance.
The team then discovered that the ability of the mesenchymal-like melanoma cells to hide from the immune system is dependent on a molecule called TCF4. Complementary to prior research which identified a therapeutic strategy that efficiently targets this particular molecule, the team demonstrated that this approach can be used to sensitize refractory melanoma to ICB in preclinical models.
Jean-Christophe Marine, VIB-KU Leuven Center for Cancer Biology: “Thanks to modern sequencing technologies, we are now able to understand the complexity of tumors like never before. We can finally track and trace each cell within a tumor and identify those cells responsible for hampering the effects of immunotherapy. By zooming in on the biology of these cells through mechanistic studies and preclinical work, we can take it a step further and search for strategies to suppress those cell types in hopes of increasing therapy efficacy. Our discovery holds great promise for melanoma patients because findings of this study could pave the way for new treatment concepts desperately needed for patients that don’t respond to immunotherapy.
The findings of this study suggest that repurposing an epigenetic drug (such as BET-inhibitors) to target the TCF4 gene may offer a viable solution to enhance patients’ sensitivity to immunotherapy. However, more research and clinical trials will be necessary to validate these findings and assess the effectiveness of the proposed treatment strategy.
The research described in this paper was possible thanks to the altruism and bravery of the melanoma patients participating in this study, and funding bodies such as the VIB Grand Challenges Program, FWO, the Marie Sklodowska-Curie fund, and Stichting tegen Kanker.
Publication
A TCF4-dependent gene regulatory network confers resistance to immunotherapy in melanoma. Pozniak et al. Cell, 2024. DOI: 10.1016/j.cell.2023.11.037
Joran Lauwers
About the VIB Grand Challenges Programma
Science can make great contributions to societal progress and increased well-being. To further stimulate the development of socially impactful scientific advances, VIB has established the VIB Grand Challenges Program. Through the ‘grand challenges strategy’, VIB seeks to support and stimulate global, transdisciplinary, multi-institutional collaborative projects. In each of these projects, various VIB groups collaborate with several external partners from universities and university hospitals across Flanders and beyond. This form of cooperation ensures that new hypotheses can be tested starting from observations, issues and needs out of practice, leading to new insights that can concomitantly be validated in a clinical setting with the final aim to result in benefits for patients.
More info can be found on https://vib.be/en/research-and-impact/grand-challenges
About UZ Leuven
More than a hospital, UZ Leuven is a university hospital where patients can count on specialised care and innovative treatments, combined with humane attention and respect for every person. Every day, more than 10,000 passionate employees provide the best possible custom-made care. Future care providers and employees receive high-quality training in UZ Leuven, with a view lifelong learning and innovation. As a pioneer in clinical research, the hospital also contributes to future patient care.