The signal that tells breast cancer cells to travel
Breast cancer became the world's most diagnosed cancer in 2021. While survival rates are high, metastasis can reduce these drastically. New research by the team of Prof. Dr. Sarah-Maria Fendt (VIB-KU Leuven Center for Cancer Biology) and international partners shows how changing levels of the protein PHGDH enable breast cancer cells to travel through the body. The results appear in the leading journal Nature.
Statistics
- Belgium has one of the highest rates of breast cancer in the world – 1 out of every 8 women receives the diagnosis at some point. (from the Global Cancer Observatory)
- The 5-year survival rate for localized breast cancer in Western societies is very high, but this drops to below 30% when the cancer spreads to distant body parts. (from the American Cancer Society)
- Yearly more than 680.000 women die from metastatic breast cancer worldwide
Stay or go?
To become truly dangerous, breast cancer cells do two things: they reproduce locally and they spread throughout the body. This last process is known as metastasis. It is, however, not always clear how cancer cells switch from staying in place to traveling through the body to affect distant organs.
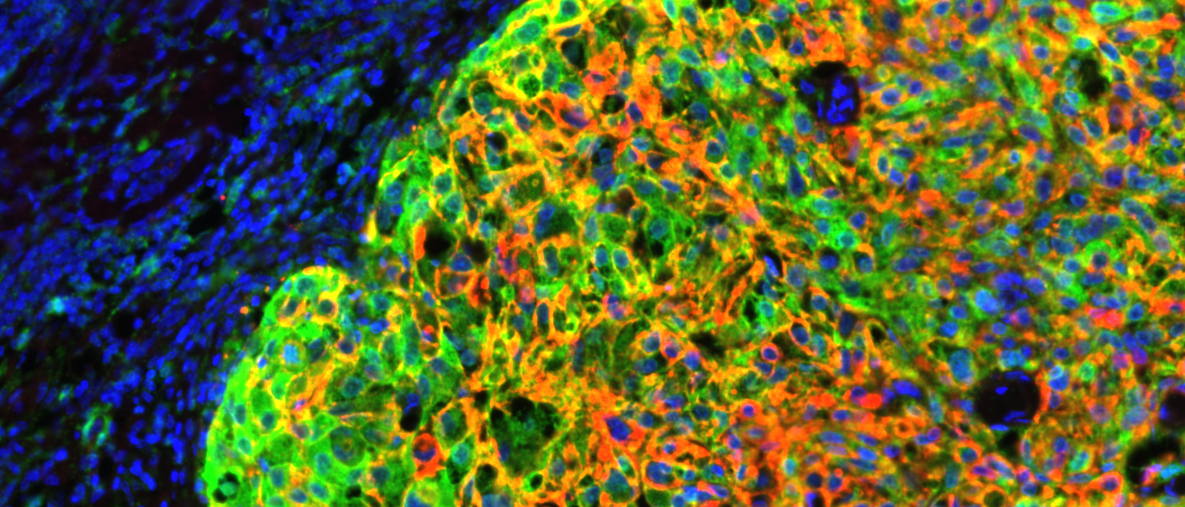
Now, work by the team of Prof. Dr. Sarah-Maria Fendt (VIB-KU Leuven Center for Cancer Biology), reveals that low levels of a protein known as PHGDH enable breast cancer cells to metastasize. The study involved a large collaboration with colleagues other labs withing the center: professors Jan Cools, Diether Lambrechts, Jean-Christophe Marine, Massimiliano Mazzone, and Peter Carmeliet, as well as international partners.
Fendt: "We know that there is quite a bit of heterogeneity in the metabolism of cancer cells, but this is relatively understudied. Here, we find that in breast cancer patients, lower levels of PHGDH expression in primary tumors are associated with a higher chance of metastasis. This suggests that metabolic processes contribute significantly to the aggressiveness of certain cancers."

High or low?
What happens is that the loss of PHGDH kickstarts a pathway that eventually changes the chemical structure of molecules on the surface of cancer cells. This, in turn, enables the cell to travel easier.
The researchers then show that targeting this chemical change (sialylation) in the surface molecule (integrin αvβ3) can decrease the metastatic capacity of cancer cells. Treating cancer cells in a cell culture with a compound that blocks sialylation reduced the number of traveling cancer cells.

Previous research had already shown that high levels of PHGDH help cancer cells proliferate locally, but this is the first time anyone describes an important effect of how PHGDH levels influence a cancer cell’s ability to metastasize.
Dr. Matteo Rossi, co-first author of the study: "Our work clarifies that there are changes in PHGDH level that are very important. This adds a new level to our understanding of the role of this protein in cancer.” Dr. Patricia Altea-Manzano, co-first author, adds: “It's not enough to focus on high or low levels, but why cancer cells can change from high to low and vice versa at different disease stages."
PHGDH heterogeneity potentiates cancer cell dissemination and metastasis.
Rossi, Altea-Manzano, et al. Nature 2022
Questions from patients
A breakthrough in research is not the same as a breakthrough in medicine. The realizations of VIB researchers can form the basis of new therapies, but the development path still takes years. This can raise a lot of questions. That is why we ask you to please refer questions in your report or article to the email address that VIB makes available for this purpose: patienteninfo@vib.be. Everyone can submit questions concerning this and other medically-oriented research directly to VIB via this address.
Gunnar De Winter